Table of Contents
- What is a PICC line? – A safe alternative to traditional intravenous vascular access
- What is a PICC line used for?
- PICC line Vs Midline catheter – what are the differences?
- Advantages of a PICC:
- Advantages of a midline:
- PICC vs Port (Portacath, Chemo port)?
- PICC line removal vs Port removal
- PICC and Midline catheter placement
- PICC Line care and Dressing change
- PICC line Dressing Change
- How long can a PICC line remain in place?
- How long can a midline catheter remain in the patient?
- Can you take a shower with the PICC or midline catheter?
- Complications of PICC Lines
- PICC line associated DVT and Recommendations
What is a PICC line? – A safe alternative to traditional intravenous vascular access
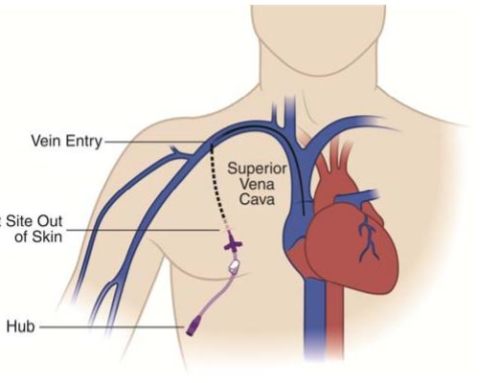
A peripherally inserted central venous catheter ( PICC or PIC line), less commonly referred to as a percutaneous indwelling central catheter, is a form of intravenous (IV) access that can be used over a longer period of time (e.g. for long term chemotherapy, extended IV antibiotic therapy, or total parenteral nutrition (TPN)) or for the administration of substances that should not be administered peripherally. Both PICC line and Midlines are catheters that enters into a peripheral vein usually on the arm through the skin (percutaneous), extends to the superior vena cava (a central vein near the heart), and can remains in place for days or weeks . First described in 1975, it is an alternative to central vein catheters which are placed through the main larger veins such as the subclavian vein, the internal jugular vein or the femoral vein in the neck and chest . The placement of subclavian and jugular lines have associated complications including a pneumothorax (air in the pleural space of the lungs), from inadvertent puncture of the lung while PICC lines have no such problem due to the method of placement.
PICCs are used for intravenous access that are more stable and allow for longer term access and outpatient care as opposed to simple IVs which cannot be left in place when patient are discharged from the hospital. PICCs allow medications to be administered closer to the heart because of the location of the tip of the catheter. This allows for administration of medication where the vessels are larger and allows for dilution of the medication being administered. This method makes it possible to intravenously administer more caustic medications which could irritate the vein walls if administered through a traditional IV which terminates in the smaller veins of the hand or forearm.
A peripherally inserted catheter that is commonly confused with a PICC is a midline catheter which is placed in a similar manner on the arm but whose tip terminates near the crease of the arm (Armpit) as opposed to a PICC. A Midline catheter is essentially a PICC that is cut short and whose tip is positioned somewhere in the arm prior to reaching the central veins near the heart. Midline catheters are generally not recommended because of the greater risk of thrombosis and venous thrombosis (DVT).
What is a PICC line used for?
Generally, PICC lines are considered when a person is expected to require more than two weeks of intravenous therapy. A PICC line can remain in place for a longer period of time than other forms of IV access, from seven days to several months as long as the line remains functional. They are used in both the hospital and the community on an outpatient basis. They are often used in people on total parenteral nutrition (TPN), chemotherapy, or long-term medications such as antibiotics. They can also be used to take blood samples. To prevent the line from clogging, the line should be periodically flushed with normal saline and “locked” by filling it with heparin or normal saline when not in use .

PICC line Vs Midline catheter – what are the differences?
PICC CATHETER
PICC stands for Peripherally Inserted Central Catheter = “peripherally inserted central venous catheter”. It is a central venous access that is introduced into the upper arm via a peripheral vein and the tip of the catheter is positioned in the superior vena cava ( superior vena cava)/Right atrium or at the cavoatrial junction . PICCs are mainly used in medium-term intravenous therapy (1 to 6 months). This makes them an excellent alternative to other central venous catheter systems, e.g. Portacath or Broviac catheter.
MIDLINE CATHETER
The midline catheter is a vascular access that is also introduced on the upper arm – but has a maximum length of approximately 25 cm. The tip of the catheter lies in a peripheral vein before getting to the level of the chest. A midline catheter is a safe alternative to IV and can remain in place longer than conventional IV (recommended for treatments 5-28 days) but are generally reserved for patients who cannot get a conventional PICC or in whom treatment requires IV access for greater than 5 days where non-caustic medication is administered. When more caustic medication such as some antibiotics and chemotherapy is to be administered a PICC is preferred because the central position of the catheter tip allows for mixing of the medication with the high blood flow near the catheter tip.
Advantages of a PICC:
PICCs are a safe and easy alternative to other central venous catheters such as Ports and broviac catheters (small bore central venous catheters), since they can also be placed on an outpatient basis by an experienced interventional specialist (e.g. doctor who has experience with image guided central venous access placement). The benefits of this type of catheter is the relative ease of placement which can be performed at bedside as compared with a port which needs to be placed in the operating room given that a skin incision and pocket has to be made to allow for the port to be implanted under the skin. Additionally infusion through a PICC is simple as is subsequent removal of the catheter which can also be done at bedside.
- Catheter can be placed at bedside for Inpatients or outpatients
- Patients can go home with PICC lines in place and have the option for outpatient infusion therapy.
- PICCs are especially favored in patients who have previously suffered a port infection
- Catheter can be left in place for medium to long terms
- New devices can confirm catheter tip position as appropriate even when the PICC is placed at bedside (port and many other catheters require xrays to confirm tip location)
- Easy removal of the catheter, which is also possible on an outpatient basis
Advantages of a midline:
For patients requiring infusion therapy of more than six days, a midline catheter is a safe alternative to an indwelling tunneled small bore central venous catheter. Midline catheters do not have to be changed regularly, and can be left on the patient for several weeks unlike peripheral IVs. This eliminates the need to repeatedly puncture the patient’s arm for IVs. Additionally, the infusion therapy can be carried out at home. Having said the benefits we generally prefer PICC lines be placed especially for those patients receiving medication which can irritate/be caustic to venous walls. The reason for this is that PICCs unlike Midline catheters have tips that terminate near the heart and allow medication to be mixed in with the high blood flow near the heart. In contrast to PICCs midline catheters tip terminates in the axilla (arm pit region) where infusion of some medications can irritate vein walls.
- Much like PICCs midline catheters can be placed at bedside for Inpatients or outpatients
- Midlines are generally reserved for those patients whom infusion duration exceeds six days.
- Outpatient infusion therapy and thus shortened hospital stay
- No x-ray is needed during placement of the midline (much like the PICC) however catheter tip does generally need to be confirmed with a post procedural xray given that devices to localize catheter tip without x ray are not widely available as they are with PICCs.
- No repeated puncture of the patient as you may need with IVs
PICC vs Port (Portacath, Chemo port)?
The PICC catheter is placed on the patient’s upper arm at bedside in a minimally invasive manner under local anesthesia (eg. local lidocaine injection). Ports on the other hand require moderate sedation or general anesthesia and have to be placed in specialized procedural rooms or an operating room. There are risks associated with moderate sedation and general anesthesia which can be avoided if a PICC can be placed. Especially in cases where port placement is not a possibility ie. Recent port site infection, the PICC catheter is a safe alternative. Medications such as chemotherapy or total parenteral nutrition can be administered via the PICC catheter or via a port.
PICC line removal vs Port removal
When it comes to removal the PICC catheter is also removed without anesthesia in the office or at bedside. Unlike the removal of a chemo port which requires moderate sedation or general anesthesia. In addition, only a small scar remains on the patient’s upper arm after the PICC catheter has been removed. In the case of ports, on the other hand, a 1-2 cm scar remains below the collarbone.
The benefits of a port on the other hand are that it is entirely implanted under the skin and can be concealed more easily. Because of this feature ports can generally remain in place longer (Years) and can be showered with as there is no external portion.
PICC and Midline catheter placement


Peripheral venous catheters are placed on the upper arm. The catheter is placed under ultrasound and using the Seldinger technique. Access into the upper arm vein is attained approximately midway between the elbow and the armpit.
After placement PICCs require an x-ray to confirm the position of the catheter tip to ensure that it is at the right atrium and superior vena cava junction also referred to as the cavoatrial junction. The position of the catheter tip can be checked either by X-rays or by devices that allow for confirmation of the tip position using EKG. In the case of midlines, position tip does not need to be confirmed as the catheter tip is positioned in a peripheral vein.
- The PICC is a peripherally inserted central venous catheter meaning that it enters a peripheral vein in the arm but the tip terminates centrally near the heart.
- The PICC is inserted into a vein of the extremity ( basilic is generally preferred, cephalic vein, brachial vein or other veins of the upper extremity), the tip of the catheter ends in the central vascular system (e.g. superior vena cava as it transitions to the right atrium commonly referred to as the cavoatrial junction).
- Only single-lumen PICCs are used at the LA Vascular because of the increased risk of DVT with multi lumen PICCs.
- The PICC is suitable for short-term or long-term therapy duration (Days-weeks-months), when evaluating a foreseeable longer duration (> 3 months) tunneled catheters or Port-A-Cath is preferred.
- The PICC is fixed with a holding plate (StatLock®) and is not generally sewn on.
PICC Line care and Dressing change
Catheter care is divided into daily and weekly care intervals.
Daily care
- Check the dressing for detachment, soiling and moisture penetration.
- Check the catheter entry point for redness, pressure sores, swelling and pain.
- If there is visible contamination, moisture penetration, leakage of fluid or signs of infection, an immediate dressing change is necessary.
- If there are signs of a catheter infection, contact your homecare service provider and / or your doctor!
- After each infusion, injection or blood sample, the catheter must then be flushed with at least 10 ml of saline (NaCl).
PICC line Dressing Change
How is a PICC or midline catheter fixed/secured onto the skin?
Peripheral venous catheters are not generally sewn/sutured on but are fixed to the skin with a special devices (e.g. StatLock). Commonly a clear (eg. Tegaderm) will be placed over the catheter entry site/StatLock to allow for better stability and visualization of the puncture site.
When should a PICC or midline catheter be flushed?
It is recommended that both types of catheters be flushed at the following times:
- After the placement
- Before and after each infusion or injection
- Before and after each blood draw
- Every 7 days even when the catheter is not in use.
How do you properly flush a PICC or midline catheter?

The catheters should be flushed with at least 10ml NaCl using the PUSH-Pause technique. With the PUSH-Pause technique, the flushing medium is applied in spurts. Syringes with a volume smaller than 10 ml should never be used on the catheters, as they build up high pressure and this can damage the catheter.
How long can a PICC line remain in place?
PICC catheters are suitable for patients who need to undergo long-term infusion therapy. Therefore, the catheters are usually used for a therapy duration that is longer than 4 weeks.
How long can a midline catheter remain in the patient?
The midline catheter is often used as a replacement for an indwelling venous cannula. It is generally used in infusion therapies that only last a few days (≤6 days).
Can you take a shower with the PICC or midline catheter?
It is possible to take a shower with the catheters if a waterproof dressing is used (e.g. Tegaderm or Dermafilm) is used. After showering, you should check whether the bandage and the puncture site have remained dry. It is therefore important that the sterile dressings used are clear. This is the only way to assess the catheter entry point.
Complications of PICC Lines
Because of the simplicity of placing central venous catheters through peripheral veins of the upper extremities, peripherally inserted central catheter (PICC) placement for various indications has become increasingly popular. Because of the way they are placed PICCs avoids complications of pneumothorax or injury to the vessels of the neck and chest, which can occur with placement of other central lines. PICCs are however associated with other important complications. The most common and concerning of which is an increased risk of deep vein thrombosis (DVT). There is some literature that suggests that PICCs are responsible for a large portion 1/3 of all upper extremity DVTs.
Incidence and Risk factors for PICC related DVT
The Michigan Risk Score can be used to assess risk of developing DVT in PICC line placement. https://www.mdcalc.com/michigan-risk-score-picc-related-thrombosis
Even when used for short-term (days) or medium-term (weeks) treatment, PICCs have a higher risk of venous thrombosis compared with centrally inserted catheters. This is especially a concern in patients who are critically ill or who have a malignancy. The incidence of deep vein thrombosis (DVT) for PICCs is between 5 and 15 percent for hospitalized patients and 2 and 5 percent for outpatients. Some studies that were set up to simply screen for even asymptomatic DVTs in patients with PICCs found as high a rate as 33%. When compared with central venous catheters PICC lines have a 2.5 fold greater risk of thrombosis among several studies reviewed.
One particular study, the Medical Inpatients and Thrombosis (MITH) Study was a case-cohort study which looked at all venous thromboembolism at a single institution from 2000 to 2009. They found that central venous catheters had a 14fold increased risk of upper extremity DVT but without significantly increased pulmonary embolism risk. Other studies have shown that repeat access into the same area further increased risk of DVT.
Risk factors for forming DVTs from PICC lines include, prior history of DVT, obesity, hematological malignancies, critical illness, and comorbidities such as diabetes and obstructive lung disease have been linked to PICC-related DVT . Additionally catheters with more lumens which are invariably larger tend to have a higher risk of DVT along with catheters placed on the left side or catheters that have been exchanged multiple times.
The catheter to the vein diameter ratio affects the risk for thrombosis. When the catheter is less than 45% the diameter of the vessel it traverses the risk of DVT decreases. PICCs that are larger than 45% the diameter of the vessel they cross have a significantly (13X) increased risk of DVT formation. The brachial and basilic veins provide a large cross-sectional area for placing a PICC. 1 study found that triple lumen PICCs were associated with a greater than 58% risk of DVT.
Other considerations include the importance of proper technique for catheter placement preferably by an interventional radiologist or someone who is well trained in placement of PICC lines. Ultrasound guidance is important in obtaining access and limiting complications. Additionally positioning of the tip of the PICC line is important in limiting complications. PICC tips should be at the cavoatrial junction or in the right atrium where blood flow is rapid and DVT risk is lessened. PICCs malpositioned with the tip in the proximal SVC have a seven fold increased risk of DVT.
Newer technique for placement of PICCs including using electrocardiographic technology (a device that localizes the PICC tip to the sinoatrial node that resides close to the cavo atrial junction/right atrium) helps position the tip of the catheter in the right spot even for bedside PICC line placement.
Clinical features and diagnosis of DVT
Most DVTs occur within the first week or two of placing the PICC line. Most of the DVTs that occur are asymptomatic. These DVTs generally occur at the junction of the axillary and subclavian veins. Symptoms often include arm or forearm pain and or swelling.
Older catheters made from silicone had higher incidence of access site issues and superficial thrombosis. These risks have decreased with the advent of polyurethane devices placed using ultrasound guidance.
Although some studies have linked DVTs in the lower extremities with placement of PICCs placed in the upper extremities the relationship is not clear. Pulmonary embolism (PE) is a rare complication with PICCs.
Diagnosis of PICC related DVT
As with most DVT, diagnosis of PICC-related DVT is made by compression ultrasonography or duplex- or Doppler-enhanced ultrasound for upper extremity . abscess of flow in the vein or non-compressibility on ultrasound helps make the diagnosis. With compression the sensitivity and specificity of ultrasound for diagnosing DVTs is above 95%. Ofcourse DVTs that are more central ie. closer to the heart cannot be seen with ultrasound and can be missed so if the ultrasound is negative but the clinical suspicion is high a ct venogram or conventional venogram can be performed.
Treating DVT related to a PICC line
Treatment includes symptomatic care, anticoagulation, and possibly thrombolysis. Symptomatic care includes extremity elevation, warm or cold compresses, and oral nonsteroidal anti-inflammatory agents (NSAIDs). Whether to remove the catheter depends on necessity for access and overall clinical picture. Replacing the PICC at a different site can run the risk of causing a second DVT at the new site.
Anticoagulation
Guidelines for the treatment of venous thromboembolism disease recommend at least three months of uninterrupted systemic anticoagulation for catheter-related upper extremity DVT (including PICC-related DVT) involving deep veins of the upper extremity (brachial, axillary, subclavian) . The type and intensity of anticoagulant therapy with catheter-related upper extremity DVT is similar to that given to prevent embolization from lower extremity DVT. While both warfarin and low-molecular-weight heparin (LMWH) may be used, LMWH is preferred in patients with catheter-related DVT who are pregnant or those with cancer.
Thrombolysis
Interventional procedures for mechanical and pharmacologic thrombolysis are well established but are reserved for large burden of thrombosis or if there is concern for phlegmasia. Indications for thrombolysis include severe symptoms that do not improve with anticoagulation, thrombosis spanning both the subclavian and axillary veins, symptoms <14 days, life expectancy >1 year, and low risk for bleeding. Catheter directed thrombolysis is usually performed with tissue plasminogen activator (tPA) over a 24 to 48 hours period. Patients are brought back after 24 hours for a check and continued for an additional 24 hours (total of 48 hours) if significant residual clot burden remains after the initial 24hrs. Angioplasty and stenting can be performed if there is significant venous outflow stenosis.
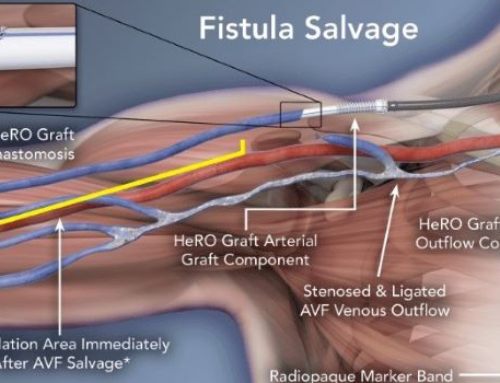
Considerations:
Phlebitis and venous stenosis can occur in patients with long standing PICCs. Patients who are dialysis dependent or may become so are better served by placing other types of centrally inserted catheters such as broviac tunneled central venous catheters. The reason for this is to save the veins in the arms which may become stenotic post PICC placement given that these veins may be used for arteriovenous fistula formation(AVF)
PICC line associated DVT and Recommendations
- Peripherally inserted central catheter (PICC) use has become increasingly popular, but PICCs are associated with a greater risk for venous thrombosis (superficial and deep veins) compared with centrally inserted catheters. Some estimates suggest that PICCs are responsible for over one-third of all upper extremity deep vein thromboses (DVTs).
- Risk factors for DVT associated with PICC placement include prior DVT, obesity, recent surgery, malignancy, critical illness, presence of certain comorbidities (eg, diabetes, obstructive lung disease, obesity), use of multilumen catheters, lack of ultrasound use for PICC placement, malpositioned PICCs and guidewire exchange of PICCs.
- Most catheter-related thromboses are clinically silent and usually occur in the first 7 to 14 days from the time of catheter placement. When symptoms do occur, patients typically complain of arm or forearm pain or swelling. The chest/upper extremity veins may dilate as collaterals develop to bypass the obstruction.
- The diagnosis of PICC-related DVT may be suspected clinically but is confirmed with vascular imaging that demonstrates venous thrombosis, typically using vascular ultrasound. Most PICC-related DVT occurs at the junction of the axillary and subclavian veins. Venography (computed tomography, catheter based) may be indicated if the diagnosis remains in question.
- The treatment of PICC-related DVT is similar to that of other catheter-related DVT and consists of symptomatic care (extremity elevation, nonsteroidal anti-inflammatory drugs [NSAIDs]) and anticoagulation for a minimum of three months. Thrombolysis can be considered for selected patients (low risk, adequate life expectancy) with PICC-related DVT who have severe symptoms (<14 days) that do not improve with anticoagulation and thrombosis spanning both the subclavian and axillary veins.
- Nonfunctional PICCs should be removed, which may help resolution of thrombosis and avoid complications (eg, bacteremia) that may occur in the setting of thrombus. For functioning PICCs, routine removal in the setting of DVT is not recommended, since reinsertion of a catheter in the contralateral upper extremity is associated with high risk of thrombosis.
- Phlebitis and inflammation of the affected upper extremity veins ultimately leads to scarring and venous stenosis. Such changes have important implications, particularly for patients with chronic kidney disease. Prior PICC placement is among the most important risk factors for hemodialysis arteriovenous vascular access failure, threatening the success of dialysis in these individuals.
- Prevention of PICC-related DVT includes :
- Avoiding use of the PICC unless it is clinically appropriate
- Ensuring appropriate catheter tip location
- Sizing of the catheter properly relative to the target vein diameter
- Removing devices promptly when they are no longer necessary



Leave a Reply