Definition: Post-infectious vasculitis of medium arteries
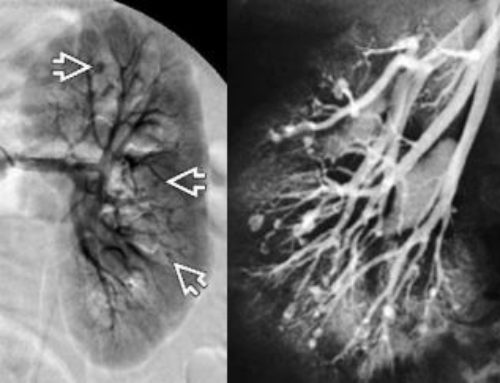
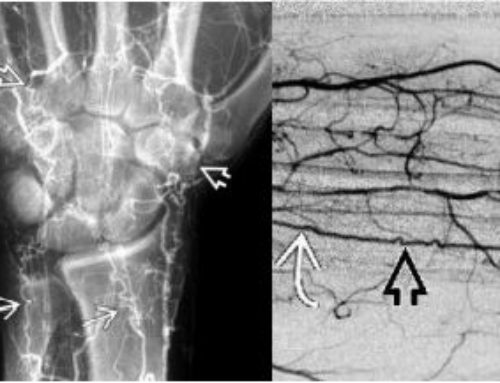
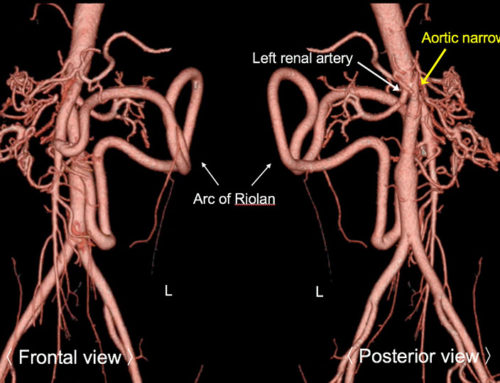
Findings: Coronary artery aneurysms (15%), conjunctivitis, rash, fever
ALSO: great vessel aneurysms
Kawasaki disease, also known as Kawasaki syndrome, is a rare autoimmune disorder that primarily affects children under the age of 5. The disease is characterized by inflammation of the blood vessels, particularly those in the heart, and can lead to serious complications, such as heart attack or stroke.
Symptoms of Kawasaki disease typically develop in three phases. In the first phase, individuals may experience a fever that lasts for more than five days, along with rash, swollen lymph nodes, and red eyes. In the second phase, which typically occurs after the fever has subsided, the individual may develop a red, peeling rash on the hands and feet. In the final phase, the disease can cause inflammation of the coronary arteries, which can lead to heart attack or other complications.
The cause of Kawasaki disease is not fully understood, but it is thought to be an autoimmune disorder in which the body’s immune system mistakenly attacks healthy tissue. This leads to inflammation of the blood vessels, which can cause them to become damaged or weakened.
Diagnosis of Kawasaki disease is typically made based on a combination of clinical symptoms and laboratory tests. Treatment for the disease typically involves the use of intravenous immunoglobulin and aspirin to control inflammation and prevent further damage to the blood vessels.
While there is no cure for Kawasaki disease, early diagnosis and treatment can help prevent serious complications, such as heart attack or stroke. It is important for parents to be aware of the symptoms of Kawasaki disease and to seek medical attention if their child develops a fever that lasts for more than five days.
SUMMARY
●Kawasaki disease (KD, also called mucocutaneous lymph node syndrome) is one of the most common vasculitides of childhood. KD occurs only rarely in adults. It is typically a self-limited condition, with fever and manifestations of acute inflammation lasting for an average of 12 days without therapy.
●KD is characterized by systemic inflammation manifested by fever and mucocutaneous involvement, including bilateral nonexudative conjunctivitis, erythema of the lips and oral mucosa, rash, extremity changes, and cervical lymphadenopathy. These findings are often not present at the same time. Thus, repeated histories and physical examinations are important in making a timely diagnosis of KD in children with fever and signs of mucocutaneous inflammation.
●Infants and possibly adults are more likely to present with incomplete KD. Infants are at greater risk for cardiovascular sequelae, possibly due in part to a delay in diagnosis and intervention. Thus, infants six months of age or less with unexplained fever for at least seven days should be evaluated for KD, even if they have no clinical findings of KD.
●No laboratory studies are included among the diagnostic criteria for typical KD. However, the presence of compatible laboratory features strongly supports the diagnosis.
●The diagnosis of KD according to classical criteria requires the presence of fever ≥5 days, combined with at least four of the other five signs of mucocutaneous inflammation, without any other explanation. A significant proportion of children with KD have a concurrent infection; therefore, ascribing the fever to such an infection or to KD requires clinical judgment. Additional clinical and laboratory features are often used to guide diagnosis in children who have fewer than five criteria for KD (incomplete KD).
●KD is most commonly confused with infectious exanthems of childhood. The presence of clinical features not commonly found in KD, including exudative conjunctivitis, exudative pharyngitis, discrete intraoral lesions, bullous or vesicular rash, splenomegaly, and/or generalized lymphadenopathy, suggest another diagnosis . Nonetheless, KD is sufficiently pleomorphic that none of these findings can definitively exclude the diagnosis. Children with KD can have concurrent infections, particularly with viruses circulating in the community at the time of their diagnosis.
Sundel RP. Kawasaki disease. Rheum Dis Clin North Am. 2015;41(1):63-73, viii. doi: 10.1016/j.rdc.2014.09.010. PMID: 25399940.

Leave a Reply