Table of Contents
Introduction
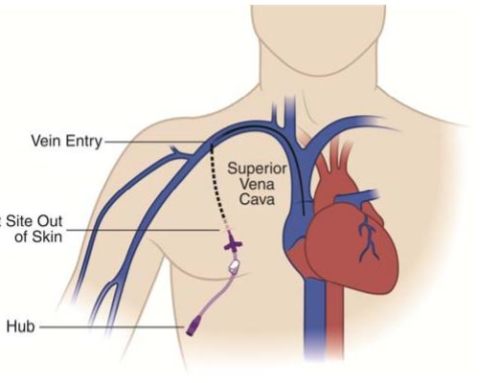
A permcath (Also known as a permacath) is a long, flexible tube (catheter) that is inserted into a vein most commonly in the neck (internal jugular vein) and less commonly in the groin (femoral vein) but that is actually tunneled under the skin and exits usually on the leg or mid thigh. This type of central venous catheter is tunneled under the skin for a few centimeters usually on the chest before it enter the neck vein. This is done when the catheter is going to be in place for long term (ie. usually greater than two weeks). If the catheter is not being left in long term then a Vascath/Quinton can be placed. A vascath/quinton catheter are non-tunneled central venous catheter that directly enters the neck or groin vein without being tunneled under the skin. The reason for the tunneling of the permacath is that it had been shown that catheters that are tunneled under the skin before entering the vein have a lower risk of becoming infected or colonized by bacteria. This benefit of tunneled permcaths is partly due to the tunneling under the skin but is also due to the fact that permacaths along with all tunneled catheter have a cuff, which is not visible and is positioned in the tunnel under the skin allowing the subcutaneous tissue to grow into the cuff essentially creating a barrier for bacteria. This cuff once in place is also responsible for keeping the catheter stable so that it does not easily slide as well as protecting it from infections.
What is a permacath?
A permacath is a name for a tunneled hemodialysis catheters — Tunneled dialysis catheters are generally double-lumen catheters with a polyester cuff positioned 1 to 2 cm from the skin exit site usually on the chest. Catheters are generally composed of silicone and other polymers, like thin polyurethane, which are less thrombogenic than the materials used in non-tunneled catheters. These catheters are blunt, soft, and more flexible than non-tunneled catheters often referred to as Quinton catheters or Vascaths.
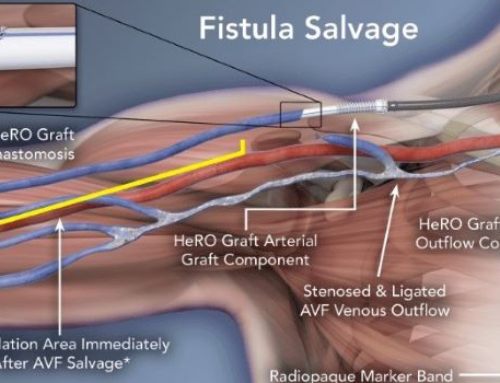
These tunneled central venous catheter can be left in place for as long as one year and provide permanent access in patients. However despite being considered permanent the longer they are in place the greater the risk that they will eventually become infected. This is why most physicians will try to use these catheters as a bridge for finding other means of even more permanent dialysis such as an arteriovenous fistula or graft which are connections surgically placed between an artery and vein usually starting out on the left forearm to allow for high blood flow and direct puncture with needles to allow for dialysis.
Permacaths although they appear to be one tube actually have two hollow bores. One part of the tube is responsible for carrying the blood to the dialysis machine and the other one carries it back from the machine to the body.
Tunneled hemodialysis catheters are associated with lower rates of infectious complications compared with non-tunneled catheters. The hemodialysis catheter is generally placed so that the cuff is positioned subcutaneously 1 to 2 cm from the skin exit site. Tissue ingrowth into the cuff seals off the catheter tunnel to reduce the risk of infection. Tunneled hemodialysis catheters are primarily used for intermediate- or long-term hemodialysis vascular access. Although chronic hemodialysis using an arteriovenous (AV) access is preferred, some patients are poor candidates for AV access creation and will require a hemodialysis catheter long term. Placement of a tunneled catheter, rather than a nontunneled catheter/Quinton/Vas Cath, is advised for patients with acute kidney injury when it is known that dialysis is likely to be for more than one week (or permanent)
A wide variety of hemodialysis catheters are available from multiple manufacturers. Tunneled catheters are available in a larger size (15.5 or 16 Fr) that allows for greater blood flow rates (>300 mL/minute) compared with nontunneled catheters (largest 13.5 Fr). Catheters are available in a variety of configurations and tip designs, including double D, coaxial, shotgun, step tip, symmetric, and split tip, among others. The differing designs are claimed to increase blood flow, minimize recirculation, and prevent catheter tip obstruction. Separation of the tips of the catheter can be achieved with a staggered tip design, use of a septum extruding beyond the openings, or splitting the catheter lumens distally. Some catheters are self-centering with a built-in curvature designed to push the tip of the catheter away from the wall of the vessel or heart chamber. Despite the wide variety of designs of tunneled hemodialysis catheters, each with its theoretical advantages and disadvantages, the few available randomized trials have failed to show the superiority of one catheter over another, particularly when the endpoint is long-term functional survival of the catheter.
Surface coated dialysis catheters
A variety of surface coatings (eg, heparin, silver, chlorhexidine, rifampin, minocycline) have been used to prevent hemodialysis catheter thrombosis and hemodialysis catheter-related infection. While nonhemodialysis catheters with antithrombotic or antimicrobial coatings have demonstrated some efficacy, few studies are available for hemodialysis catheters, and those that are available provide only short-term outcomes.
In early studies, antimicrobial- and antithrombogenic-coated hemodialysis catheters appeared to be effective in preventing intravascular catheter infections in the dialysis setting. However, in a systematic review that evaluated 29 trials with 2886 patients and 3005 hemodialysis catheters, the incidence of catheter-related bacteremia and exit-site infections was similar for antimicrobial-coated hemodialysis catheters compared with noncoated catheters .
Heparin-coated catheters have also been used to decrease the incidence of catheter-related thrombosis. In observational studies, the frequency of catheter malfunction and overall catheter survival was similar. While the incidence of catheter-related bacteremia was significantly less frequent for heparin-coated catheters compared with noncoated catheters (34 versus 60 percent), infection-free catheter survival was no different. It is important to remember that hemodialysis catheters remain in the patient for several months, which is a critical factor when determining the efficacy of a coating. Randomized trials are needed to demonstrate the longevity of any bonded protection, which ideally should approximate the length of the intended catheter placement. Also, it is important to establish whether any effect remains in settings in which infection preventive care is established and adhered to. In the absence of reliable data demonstrating long-term efficacy, these catheter are not broadly recommended.
Hemodialysis catheter life
The overall survival of tunneled hemodialysis catheters is highly variable. Unassisted one-year use-life (ie, no intervention) of tunneled hemodialysis catheters appears to be as low as 9 percent, but reports are not consistent. Assisted one-year use rates range between 25 and 93 percent. One study reported a 74 percent one-year and a 43 percent two-year catheter survival. A larger study of 623 Tesio catheters (Long term tunneled hemodialysis catheters) reported the one-year and three-year postplacement use-life of 78 and 44 percent, respectively. In another study, assisted one-year patency was 50 percent when the catheter was used as a permanent access. Almost all catheter losses were due to bacteremia.
Indications for permacath placement
Permcath (Permacath), better known as a tunneled dialysis catheter or long term hemodialysis catheter is used in a variety of cases. Here are a few indications;
- Regular hemodialysis to treat kidney failure in an outpatient setting – permacath avoids some of the high infectious risks of non-tunneled hemodialysis catheters and serves as a permanent catheter for dialysis.
- Route/access for plasmapheresis.
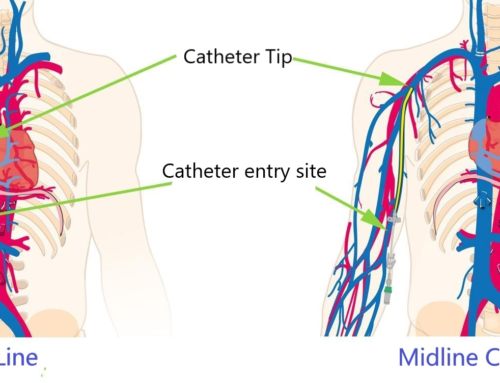
- Frequent blood sampling/infusion in an outpatient setting although other catheters are preferred for this including PICC lines, Portacaths and broviac catheters.
- Administration of drugs and fluids during long-term treatment in very specific settings (more commonly used catheters in this setting include PICC lines, Portacaths and broviac catheters)
- Administration of caustic medications (chemotherapy) that may harm peripheral veins although the preferred methods of administering these drugs include PICC lines, Portacaths and broviac catheters some centers reportedly use permacaths
- A route for TPN and blood products in special cases where smaller bore catheters such as hickman catheters are not able to be used
Permacath placement
Local anesthesia and ultrasound guidance should be used for nontunneled hemodialysis catheters also known as Vascath/Quinton catheters. These non-tunneled catheters can be placed at the bedside or in a procedure room. Confirmation of the catheter tip position must be documented using fluoroscopy or chest film prior to use of the catheter. Tunneled catheters like permcaths (permacaths) are placed with ultrasound and fluoroscopic guidance using local anesthesia, with or without sedation, in an angiographic suite or appropriately equipped operating room due to their larger caliber and the need to tailor the catheter for proper positioning. Catheter malposition is a common problem (25 to 40 percent) when fluoroscopy is not used for guidance; accurate catheter positioning can be achieved in 95 to 100 percent of cases with fluoroscopy. Fluoroscopy also allows direct imaging of the wires and dilators to minimize the potential for injury.
Local anesthesia and ultrasound guidance should be used for nontunneled hemodialysis catheters and can be placed at the bedside or in a procedure room. Confirmation of the catheter tip position must be documented using fluoroscopy or chest film prior to use of the catheter. Tunneled catheters are placed with ultrasound and fluoroscopic guidance using local anesthesia, with or without sedation, in an angiographic suite or appropriately equipped operating room due to their larger caliber and the need to tailor the catheter for proper positioning. Catheter malposition is a common problem (25 to 40 percent) when fluoroscopy is not used for guidance; accurate catheter positioning can be achieved in 95 to 100 percent of cases with fluoroscopy. Fluoroscopy also allows direct imaging of the wires and dilators to minimize the potential for injury.
Where is a Permacath placed?
As with any central venous catheter, hemodialysis catheters can be inserted into any of the central veins. The choice of the vascular access site and catheter should be guided by the urgency of dialysis, type of dialysis, history of prior access, and the overall medical condition of the patient.
The right internal jugular vein is the preferred vein for hemodialysis access (nontunneled and tunneled hemodialysis catheters) because the vein takes a straight path directly into the superior vena cava. Placement of catheters into the left internal jugular vein requires that the catheter make two right angles prior to reaching the superior vena cava, which can cause difficulties during insertion, and there is a higher incidence of catheter dysfunction, particularly with nontunneled hemodialysis catheters In a retrospective review of 532 catheters, left-sided internal jugular vein catheters also had higher rates of infection (0.50 versus 0.27) and dysfunction (0.25 versus 0.11) compared with those inserted from the right.
Common femoral vein hemodialysis catheter insertion may be needed, particularly in the setting of bilateral occlusion of the central thoracic veins. Venous access at the common femoral vein avoids many of the complications associated with thoracic central venous access (eg, pneumothorax, air embolism). In a French trial of 750 intensive care unit patients requiring acute renal replacement therapy, there was no significant difference in infection rates between jugular and femoral access, but there was a higher rate of hematoma in the jugular group.
A longer catheter is needed when hemodialysis access is placed into the common femoral vein. A catheter length greater than 24 cm (tip to hub) is adequate for most average-sized adults to position the tip of the catheter in the inferior vena cava. Short hemodialysis catheters (less than 15 cm long) have higher recirculation rates when the tip of the catheter is positioned in the iliac vein.
The subclavian vein, although not a preferred site, can also be used for tunneled catheters if the jugular veins are occluded and the common femoral vein is not a good option. However, this site has a high incidence (15 to 50 percent) of subclavian vein stenosis and subclavian vein thrombosis, and in general, subclavian vein insertion sites should be avoided. Subclavian stenosis/thrombosis also compromises the placement of permanent ipsilateral upper extremity arteriovenous (AV) hemodialysis access.
In cases of complete occlusion or obliteration of femoral and central (neck/thoracic) veins, the femoral artery can be used if immediate access is required. In cases where central venous obstruction prevents use of typical access sites, other AV access techniques (eg, sharp needle recanalization) can be used. Advanced percutaneous approaches for catheter placement (eg, translumbar, transhepatic) are possible if no alternative form of AV access is possible. Advanced surgical approaches used can place a catheter directly into the right atrium, superior vena cava, inferior vena cava, or azygos vein. More complicated approaches are associated with increased technical difficulty and morbidity.
How is a Permacath placed? – technique
After obtaining appropriate informed consent, hemodialysis catheters are inserted percutaneously using a modified Seldinger guidewire technique. Catheter placement using ultrasound guidance is recommended and is the accepted standard for internal jugular and femoral catheter placement. Technical success and reduced rates of access-related complications correlate with experience and the use of ultrasound guidance. Specific techniques to facilitate placement of central catheters at the jugular, femoral, and subclavian access sites are discussed in detail elsewhere.
Preventing infection related to hemodialysis catheters requires adherence to strict technique and optimal catheter management. Measures to minimize hemodialysis catheter infection, including the use of antimicrobial agents at the exit site, antibiotic lock solutions, and eradicating nasal carriage, are discussed elsewhere.
For tunneled catheters, the insertion technique varies depending upon the type of catheter. In general, tunneling the catheter follows venous puncture and guidewire placement. Because of the large diameter of hemodialysis catheters, a valved introducer peel-away sheath is needed to deliver the catheter into the vessel after dilation of the overlying soft tissues. The dilators and sheaths are stiff and should be imaged during their placement using fluoroscopy to ensure that the tip of the dilator is not taking an aberrant path, deforming the wire, or pushing through the vessel. This is particularly important in patients who have been hemodialysis dependent for an extended period and who may have central venous occlusive pathology as a result. Specific techniques for placing tunneled catheters are discussed in detail elsewhere.
Ultrasound guidance — Real-time ultrasound guidance is recommended for venous access during the placement of central venous catheters. Appropriate training is required to effectively use ultrasound devices.
Ultrasound is used to assess vein size and patency prior to venous puncture. In a study of 143 hemodialysis patients with a history of prior hemodialysis catheter placement, 25.9 percent had jugular vein thrombus and 62 percent of these occluded. Ultrasound guidance during venipuncture minimizes the incidence of venous access-related complications, decreases procedure time, and increases the rate of initial technical success. Ultrasound-guided venous access also decreases the likelihood of arterial puncture or pneumothorax in patients undergoing hemodialysis catheter placement. In a meta-analysis, ultrasound guidance significantly decreased the risks of hemodialysis catheter placement failure (relative risk [RR] 0.12, 95% CI 0.04-0.37), failure to place catheter on first attempt (RR 0.40; 95% CI 0.29-0.56), arterial puncture (RR 0.22, 95% CI 0.06-0.81), and access site hematoma (RR 0.27, 95% CI 0.08-0.88). Another advantage of an ultrasound-guided technique in placing internal jugular hemodialysis catheters is that it allows the vein to be punctured more caudally (closer to the clavicle), which may reduce kinking; even a minimal degree of kinking can severely diminish flow rates.
Catheter positioning — Prior to the use of a central catheter for hemodialysis, the positioning of the tip of the catheter needs to be verified, typically using fluoroscopy or plain radiography.
Ideal positioning of hemodialysis access catheters is as follows:
●The tip of nontunneled jugular hemodialysis catheters/Vascath/Quinton should be positioned in the distal superior vena cava. Because of the stiffness of short-term access catheters and risk for complications, atrial placement should be avoided .
●When placed with the patient supine, the tip of tunneled hemodialysis catheters should be positioned within the right upper atrium. As the patient transitions to the upright position, the catheter will tend to retract 2 to 4 cm. Retraction of the catheter is greater for left-sided placement. If the catheter is placed too shallow, it may end up positioned in the superior vena cava or brachiocephalic vein (particularly in obese patients or large-breasted women), which can lead to a catheter malfunction. In a retrospective review of 532 internal jugular hemodialysis catheters, left-sided catheters terminating in the superior vena cava or peri-cavoatrial junction had significantly more episodes of catheter dysfunction or infection compared with left-sided catheters terminating in the mid- to deep right atrium (0.84 versus 0.35), whereas no significant difference was identified for right-sided catheters based on tip position.
●The tip of femoral hemodialysis catheters (nontunneled or tunneled) should be placed in the inferior vena cava proximal to any stenotic lesions to minimize recirculation. Iliac vein positioning must be avoided. Since many nontunneled catheters are relatively short, placement of a tunneled catheter may be necessary to obtain appropriate length to enable adequate hemodialysis.
Permacath (permcath) removal
Permacath removal is generally considered a simpler procedure than the placement of the catheter and does not require imaging. Removal of a permcath along with all tunneled central venous catheters can be performed at bedside. Indications of permacath removal are;
- Access no longer required, either due to completion of renal treatment or due to the availability of a better alternative
- Catheter related infection that is not amenable to antibiotic treatment (Pseudomonas infections or pus seen coming from the catheter entry site are relatively common reasons to remove catheters)
- Persistent catheter infection (Most catheter infections are treated with antibiotics initially. We dont advocate for reflexive catheter removal in the setting of an infection. the entire clinical picture has to be considered along with the fact that removing a hemodialysis catheter in a patient who will need access for dialysis will require replacement of the dialysis catheter at a different site which can increase risk of vein occlusion and stenosis.
- Damaged or inappropriately functioning catheter. Although rare catheter cuffs can put out of the tract requiring replacement as the cuff acts as a infection barrier that when dislodged no longer provides an infection barrier function.
Removal of tunneled dialysis catheter requires sterile technique and local anesthesia such as lidocaine generally injected at the catheter entry site near the chest and around the subcutanous cuff. This is followed by cutting the retention suture (A suture placed at the catheter exit site on the the chest) if it is still in place . Then attention is directed at providing gentle traction to the catheter while dissecting the cuff of the tunneled hemodialysis catheter which is a few cm from the catheter exit site from the subcutaneous tissues. Sedation is seldom necessary. Some tunneled catheters which have been in place for a week or less have not had time for the cuff to grow into the subcutaneous tissues and can be removed by simply cutting the retention suture (A suture placed at the catheter exit site on the the chest) and gentle traction.
On occasion the catheter cuff is positioned at a very deep site or the catheter has what is called a fibrin sheath or other issue which can make simple removal difficult if not impossible. in these cases a cut down or second incision along the length of the catheter is required. This is a very rare occurrence.
Permcath (permacath) complications
There are a number of complications that may occur during placement of this permanent catheter for dialysis. However, a professional could avoid most of these by following proper protocol and aseptic techniques. These complications are;
- Arterial puncture (much less likely under ultrasound guidance)
- Pneumothorax on occasion if a lung is punctured during placement (Very rare)
- Hemothorax which is blood around the lung which can occur with incorrect puncture of an artery or rupture of a vein (Very very rare)
- Pain
- Cardiac arrhythmias which can be common during the procedure while wires are being passed through the heart. this is almost always self limited and stops once the wires are repositioned
- Air embolism – a life threatening complication which was much more common in older catheter designs (non-valved peel away sheaths)
- Bleeding
- Cardiac tamponade – blood pooling in the pericardial space which can occur with a rupture of a vein
Permcath (permacath) care
With a permacath in place, you need to be cognizant of its position especially while rolling in bed or during vigorous activities that can result in pulling of the catheter. Another consideration is that you have to make sure that the dressing over the catheter entry site is always clean and dry. A short shower with the catheter site covered is preferred to a bath which we do not recommend given the theoretically increased risk of infection with a submerged incision site. The dressing should always be dry and secure, so that along with the suture and cuff it holds the catheter in position firmly and acts as a barrier to infection.
Along with these recommendations make sure you abide by your providers instructions and go through the guidelines thoroughly in order to avoid infection risk. If you feel pain, swelling, redness or any other unusual symptom, contact the doctor immediately.
Catheter dressing — After catheter placement some centers will prime catheters with high dose heparin which is a blood thinner and will prevent clotting of the catheter but some catheters may use other products such as alcohol or saline. Before a dialysis session the dressing is usually removed and the heparin/alcohol or saline is withdrawn after which the catheter can be used. After completing dialysis each lumen of the catheter is then filled with a lock solution as mentioned and a new dressing is placed.
The exit site of the catheter is redressed with a sterile bandage and antimicrobial ointment applied for at least the first two to three weeks following insertion. A variety of other agents have been used at the exit site to prevent infection.


A great explanation. Very thorough thank you!
Thank you. I’m going to have a permacath placed before I have an AV fistula surgically created down the line likely a few months from today. My surgeon has told me that I can keep the permacath in long term but just as you mentioned in the article that the catheter can get infected after some time.
If the dialysis cath is used just to draw blood which lumen should be used . Red or blue
We don’t generally recommend using a dialysis catheter for blood draws unless it is a trialysis catheter which is a dialysis catheter with a 3rd smaller lumen meant specifically for blood draws. The reason for this is the theoretical increased risk for infection with repeated use of the dialysis catheter for blood draws. For centers that still choose to draw blood from dialysis catheters knowing the above mentioned risks we recommend using the red port which identifies the “arterial” lumen because that is the port that normally draws blood from the body during dialysis.