Table of Contents
Quick Take on Temporal Arteritis/Giant Cell arteritis (GCA):
- Nomenclature: Temporal arteritis is also known as Giant cell arteritis (GCA), Horton disease, and cranial arteritis. All of these names refer to the same disease process
- Demographics: Older patients, age > 50, women > men
- Imaging features: Long, smooth stenosis of medium sized arteries: External Carotid Arteries (ECA), temporal arteries, subclavian/axillary arteries
- How the diagnosis is generally made: temporal artery biopsy
Giant cell arteritis, also known as temporal arteritis, is a chronic autoimmune disorder that causes inflammation of the arteries, particularly those in the head and neck. The disease typically affects people over the age of 50, and is more common in women than in men.
Symptoms of giant cell arteritis can include headache, scalp tenderness, fever, fatigue, and jaw pain. In some cases, the disease can cause vision loss or blindness due to inflammation of the arteries that supply blood to the eyes.
The exact cause of giant cell arteritis is not known, but it is thought to be an autoimmune disorder in which the body’s immune system mistakenly attacks healthy tissue. This leads to inflammation of the arteries, which can cause them to narrow or become blocked.
Diagnosis of giant cell arteritis is typically made based on a combination of clinical symptoms, imaging tests such as CT scans or MRIs, and blood tests. Treatment for the disease typically involves the use of corticosteroids and immunosuppressive medications to control inflammation and prevent further damage to the arteries.
While there is no cure for giant cell arteritis, early diagnosis and treatment can help prevent serious complications, such as vision loss or stroke. It is important for individuals who are at risk for the disease to be monitored by a healthcare provider and receive regular check-ups to ensure the condition is properly managed.
Temporal arteritis/giant cell arteritis (GCA)
What is temporal arteritis/giant cell arteritis (GCA)?
Giant cell arteritis, also called GCA or temporal arteritis, is a disorder in which certain arteries (blood vessels) in the body become inflamed. It frequently occurs in conjunction with polymyalgia rheumatica (PMR). About 10-15% of people with PMR also have temporal arteritis, and nearly 50% of patients with temporal arteritis also have PMR.
What are the symptoms of temporal arteritis/giant cell arteritis (GCA)?
Temporal arteritis commonly affects the arteries in the temple area (temporal region) on both sides of the head. It also involves arteries in the head, neck, arms, and occasionally other major arteries in the body. The inflammation causes the arteries to narrow or block, so that little blood passes through. The symptoms of temporal arteritis that indicate inflammation or blockage of the arteries are:
- Sore temples or scalp
- Blurred or double vision, loss of vision (this may be intermittent or with the appearance that a curtain is partially covering the eye).
- Severe headaches
- Pain in the jaw when eating or speaking
- Persistent sore throat or difficulty swallowing saliva, Cough
Giant cell arteritis/temporal arteritis can be difficult to diagnose in some people who never have headaches or scalp pain. Instead, these people may have more ambiguous symptoms such as flu, fever, fatigue, weight loss, and anemia.
Vision loss can be temporary or permanent. Early diagnosis and treatment with glucocorticoids has helped reduce the frequency of permanent blindness due to temporal arteritis.
Important: If you have polymyalgia rheumatica and begin to have vision problems, call your doctor immediately. Also tell you physician if you have any other temporal arteritis symptoms. Early diagnosis and treatment of giant cell arteritis/temporal arteritis can help prevent serious problems such as blindness.
How is temporal arteritis/giant cell arteritis (GCA) diagnosed?
To determine if you have temporal arteritis, your doctor will need to remove a sample from the temporal artery above and in front of your ear. The biopsy sample of the artery will be obtained from the temple through a small incision. Most placed perform this biopsy under moderate sedation and local anesthesia ie. You will not need to be under general anesthesia or asleep for this, but you will receive medicine to numb the area. The piece of artery sampled will be examined under a microscope. If you have temporal arteritis, the inflammation will show up on the artery walls. In rare cases, the disease cannot be detected by biopsy. The doctor will make a final diagnosis based on other symptoms and signs.
If you have temporal arteritis, you may have some lab abnormalities as well including a higher than normal coefficient of sedimentation, indicating inflammation in the body. Other tests that can be performed may show anemia, an elevated platelet count, and abnormal liver function results.
Treatment options for temporal arteritis/giant cell arteritis (GCA)
Corticosteroid medications are used to treat this condition. Higher doses are used to treat temporal arteritis than for PMR (usually 40-60 mg / day in one or two daily doses). These doses will put you at greater risk for side effects. To prevent osteoporosis, which can result from ingesting glucocorticoids, it is important to take calcium and vitamin D supplements .
Expect to be in treatment for many months to several years, although your doctor will likely reduce your dose over time once your symptoms are under control.
Prognosis of temporal arteritis/giant cell arteritis (GCA)
Both PMR and giant cell arteritis/temporal arteritis can last one to two years, but this varies from person to person. These conditions rarely recur if you have been well for some time.
Research is aimed at finding treatments focused on controlling inflammation with lower doses of corticosteroids. Current treatment allows most people with these diseases to lead active and productive lives. Most of them can take lower doses of drugs after they have been treated for a while. Many patients can eventually stop taking the drugs after a year or two, but the threat of a recurrence requires constant communication between you and your doctor.
Summary of facts for temporal arteritis/giant cell arteritis (GCA):
●The diagnosis of giant cell arteritis (GCA, also known as Horton disease, cranial arteritis, and temporal arteritis) should be considered in a patient over the age of 50 years who complains of or who is found to have one or more of the following:
•A new headache
•Abrupt onset of visual disturbances, especially transient monocular visual loss
•Jaw claudication
•Unexplained fever or anemia
•Elevated erythrocyte sedimentation rate (ESR) and/or serum C-reactive protein (CRP)
Any of these findings are of especial concern in the context of a current or previous diagnosis of polymyalgia rheumatica (PMR).
●Temporal artery biopsy remains the traditional gold standard for the diagnosis of temporal arteritis. For those who have undergone unilateral biopsy, contralateral biopsy can be considered if the first biopsy is negative and the clinical suspicion for the diagnosis of temporal arteritis remains high.
●Scheduling of temporal artery biopsy should never interfere with the initiation of treatment in a patient with a high likelihood of temporal arteritis, since delay can put the patient at risk for complications, particularly sight loss. Resolution of the inflammatory infiltrate in the temporal artery occurs slowly after the start of treatment, so an accurate diagnosis of temporal arteritis by temporal artery biopsy can be made several weeks or even months after the start of prednisone therapy.
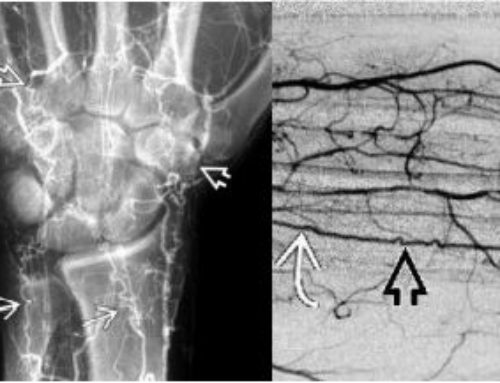
●Color Doppler ultrasonography (CDUS) can visualize the temporal arteries and, for clinicians skilled in this technique, can function as an alternative diagnostic procedure in the initial evaluation of temporal arteritis.
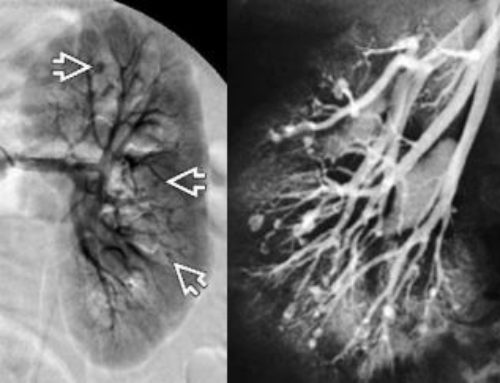
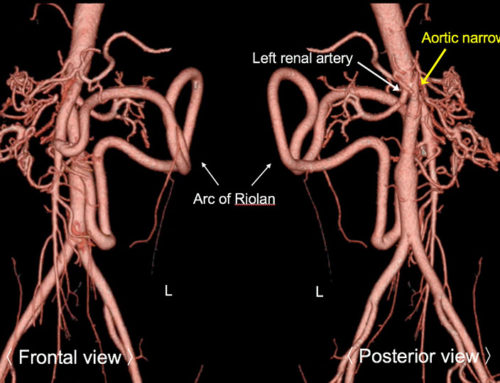
●When the diagnosis of temporal arteritis is still suspected in a patient who has had a negative temporal artery biopsy and/or CDUS, the possibility of large vessel involvement can be considered. The diagnostic procedure of choice for suspected large vessel temporal arteritis is an advanced imaging study of the torso. Computed tomography (CT) or CT with angiography (CTA), magnetic resonance imaging (MRI) or MR angiography (MRA), and positron emission tomography (PET) or PET with CT are useful for the identification of large vessel temporal arteritis/giant cell arteritis.
●The differential diagnosis of temporal arteritis includes other vasculitides (eg, Takayasu arteritis, small- and medium-sized vessel vasculitides, primary angiitis of the central nervous system), nonarteritic anterior ischemic optic neuropathy (NAAION), and infection.
References:
Ciofalo A, Gulotta G, Iannella G, Pasquariello B, Manno A, Angeletti D, Pace A, Greco A, Altissimi G, de Vincentiis M, Magliulo G. Giant Cell Arteritis (GCA): Pathogenesis, Clinical Aspects and Treatment Approaches. Curr Rheumatol Rev. 2019;15(4):259-268. doi: 10.2174/1573397115666190227194014. PMID: 30827250.


Leave a Reply