- Definition: necrotizing, small/medium-vessel vasculitis
- Symptoms: myalgias, arthralgias, subcutaneous nodules, neuropathy, hematuria
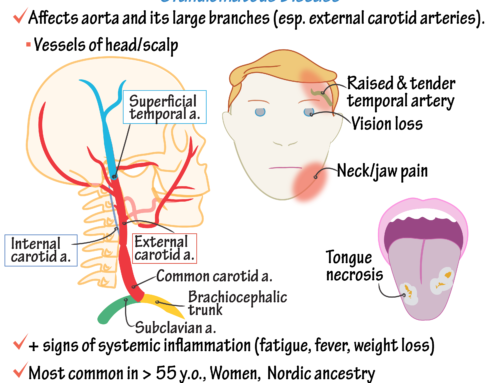
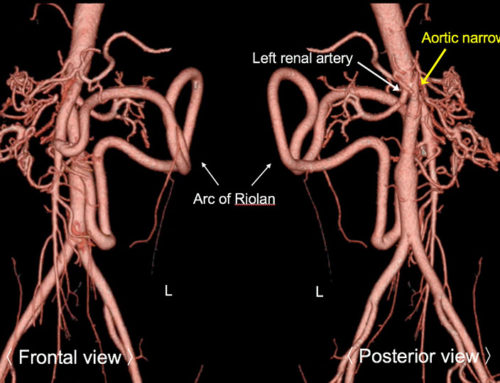
- Distribution of disease: Renal artery branches (85%) > hepatic artery branches (50%) = small mesenteric branches (50%)
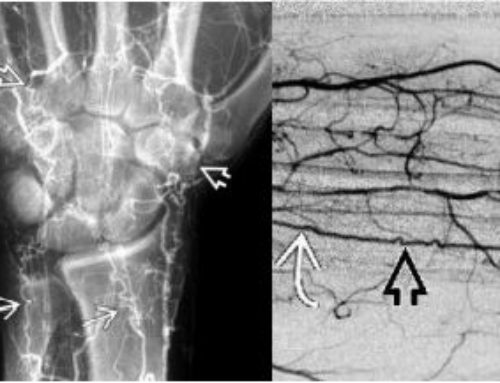
- Imaging features: microaneurysms
- Treatment: mainstay is steroids. Coiling may be helpful for larger aneurysms for risk of rupture.
- Differential diagnosis = MPA, Lupus, mycotic aneurysms (sepsis), speed kidney (methamphetamine)
Polyarteritis nodosa, or PAN, is a rare autoimmune disorder that causes inflammation of the small and medium-sized arteries. The disease can affect any organ in the body, but is most commonly associated with the kidneys, nerves, and digestive system.
Symptoms of polyarteritis nodosa can vary depending on the specific organs affected, but can include abdominal pain, fever, weight loss, and weakness. In severe cases, the disease can cause organ failure or even death.
The cause of polyarteritis nodosa is not fully understood, but it is thought to be an autoimmune disorder in which the body’s immune system mistakenly attacks healthy tissue. This leads to inflammation of the arteries, which can cause them to narrow or become blocked.
Diagnosis of polyarteritis nodosa is typically made based on a combination of clinical symptoms, imaging tests such as CT scans or MRIs, and biopsy of affected tissue. Treatment for the disease typically involves the use of corticosteroids and immunosuppressive medications to control inflammation and prevent further damage to the arteries.
While there is no cure for polyarteritis nodosa, early diagnosis and treatment can help prevent serious complications and improve outcomes for individuals with the disease. It is important for individuals who are at risk for polyarteritis nodosa to be monitored by a healthcare provider and receive regular check-ups to ensure the condition is properly managed.
SUMMARY:
●Polyarteritis nodosa (PAN) is a systemic necrotizing vasculitis that typically affects medium-sized muscular arteries, with occasional involvement of small muscular arteries. The spectrum of disease known as PAN has evolved and narrowed substantially due to the identification and classification of other forms of vasculitis that had previously been considered PAN, particularly microscopic polyangiitis (MPA). Unlike MPA, PAN is not associated with the presence of antineutrophil cytoplasmic antibodies (ANCA). The diagnosis is most commonly made in middle-aged or older adults, and the incidence rises with age, with a peak in the sixth decade of life.
●Most cases of PAN are idiopathic, although hepatitis B virus infection, hepatitis C virus infection, and hairy cell leukemia are important in the pathogenesis of some cases, which are termed secondary PAN. The pathogenetic mechanisms in PAN are poorly understood. It seems likely that, in terms of pathogenesis and pathophysiology, PAN represents a spectrum of disease rather than a single entity. Regardless of the underlying cause, established PAN is characterized by segmental transmural inflammation of muscular arteries; it does not involve veins, unlike other forms of systemic vasculitis.
●Patients with PAN typically present with systemic symptoms (fatigue, weight loss, weakness, fever, arthralgias) and signs (skin lesions, hypertension, renal insufficiency, neurologic dysfunction, abdominal pain) of multisystem involvement.
●A clinical diagnosis of PAN is suspected based upon the presence of characteristic symptoms, physical findings, and compatible laboratory test results. However, because of the relative rarity of this disease and because of the potentially severe adverse effects related to treatment, the diagnosis should be confirmed by biopsy whenever possible. In the absence of an obvious site for biopsy, angiography sometimes reveals microaneurysms of blood vessels in the renal, hepatic, or mesenteric circulations.
●The diagnosis of PAN is informed by the classification criteria developed by the American College of Rheumatology and by the definitions and nomenclature of the Chapel Hill Consensus Conference, but there are no validated diagnostic criteria for PAN. Thus, the diagnosis remains a clinical diagnosis that importantly includes exclusion of entities that mimic this rare disease.
●The differential diagnosis of PAN is broad, including infectious diseases that affect the vasculature or that are complicated by systemic vasculitis; noninfectious disorders, particularly those that can cause widespread arterial embolism, thrombosis, or vasospasm; and other systemic vasculitides.
Hernández-Rodríguez J, Alba MA, Prieto-González S, Cid MC. Diagnosis and classification of polyarteritis nodosa. J Autoimmun. 2014 Feb-Mar;48-49:84-9. doi: 10.1016/j.jaut.2014.01.029. Epub 2014 Jan 28. PMID: 24485157.


Leave a Reply