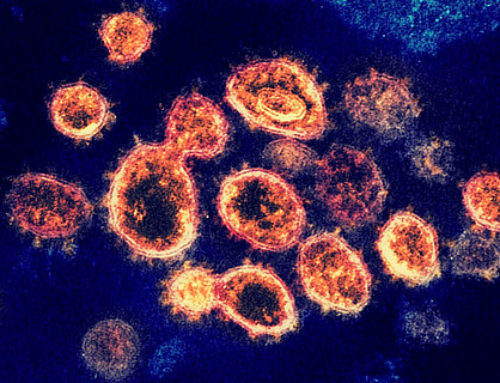
A. Observations of “acquired immunity” to diseases and primitive vaccination practices
contributed to our understanding of the immune response to infectious agents and the design of passive and active immunization strategies.
INTRODUCTION
Routine immunization schedules vary from country to country. This topic will provide an overview of immunization for children and adolescents in the United States. Immunization schedules for other countries are available through the World Health Organization.
BENEFITS OF VACCINES
Immunization is one of the most effective preventive health measures. The number of cases of most vaccine-preventable illnesses in the United States declined by more than 90 percent after routine childhood immunizations were introduced.
Vaccination programs directly benefit the immunized child. They also indirectly benefit unimmunized persons through community (“herd”) immunity. Community immunity occurs when the portion of the population that is immune to the infection is large enough to decrease the risk of transmission. Community immunity protects children who are too young for immunization and persons with contraindications to vaccines. It relies on the majority of the population receiving routinely recommended immunizations.

This schedule is recommended by the Advisory Committee on Immunization Practices (ACIP) and approved by the Centers for Disease Control and Prevention, American Academy of Pediatrics, American Academy of Family Physicians, American College of Obstetricians and Gynecologists, and the American College of Nurse-Midwives.
- Consult relevant ACIP statements for detailed recommendations.
- When a vaccine is not administered at the recommended age, administer at a subsequent visit.
- Use combination vaccines instead of separate injections when appropriate.
- Report clinically significant adverse events to the Vaccine Adverse Event Reporting System (VAERS) online at https://vaers.hhs.gov or by telephone, 800-822-7967.
- Report suspected cases of reportable vaccine-preventable diseases or outbreaks to your state or local health department.
- For information about precautions and contraindications, refer to https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html.
- For information regarding vaccination in the setting of a vaccine-preventable disease outbreak, contact your state or local health department.
* School entry age group.
¶ Hepatitis B (HepB) vaccine
(Minimum age: Birth)
- Birth dose (monovalent HepB vaccine only):
- Mother is hepatitis B surface antigen (HBsAg)-negative: 1 dose within 24 hours of birth for all medically stable infants ≥2 kg. Infants <2 kg: Administer 1 dose at chronologic age 1 month or hospital discharge.
- Mother is HBsAg-positive:
- Administer HepB vaccine and 0.5 mL of hepatitis B immune globulin [HBIG] in separate limbs) within 12 hours of birth, regardless of birth weight. For infants <2 kg, administer 3 additional doses of vaccine (total of 4 doses) beginning at age 1 month.
- Test for HBsAg and hepatitis B surface antibody at age 9 through 12 months. If HepB series is delayed, test 1 to 2 months after final dose.
- Mother’s HBsAg status is unknown:
- Administer HepB vaccine within 12 hours of birth, regardless of birth weight.
- For infants <2 kg, give 0.5 mL of HBIG in addition to HepB vaccine (in separate limbs) within 12 hours of birth. Administer 3 additional doses of vaccine (total of 4 doses) beginning at age 1 month.
- Determine mother’s HBsAg status as soon as possible. If mother is HBsAg-positive, administer 0.5 mL of HBIG to infants ≥2 kg as soon as possible, but no later than 7 days of age.
- Routine vaccination:
- Three-dose series at ages 0, 1 through 2, and 6 through 18 months (use monovalent HepB vaccine for doses administered before age 6 weeks).
- Infants who did not receive a birth dose should begin the series as soon as feasible. Refer to UpToDate content related to the catch-up schedule.
- Administration of 4 doses is permitted when a combination vaccine containing HepB is used after the birth dose.
- Minimum age for the final (third or fourth) dose: 24 weeks.
- Minimum intervals: Dose 1 to dose 2: 4 weeks; dose 2 to dose 3: 8 weeks; dose 1 to dose 3: 16 weeks (when 4 doses are administered, substitute “dose 4” for “dose 3” in these calculations).
- Special situations:
- Revaccination is not generally recommended for persons with a normal immune status who were vaccinated as infants, children, adolescents, or adults
- Revaccination may be recommended for certain populations, including infants born to HBsAg-positive mothers, hemodialysis patients, and other immunocompromised persons.
Δ Rotavirus (RV) vaccine
(Minimum age: 6 weeks)
- RV1 (Rotarix): 2-dose series at ages 2 and 4 months.
- RV5 (RotaTeq): 3-dose series at ages 2, 4, and 6 months.
- If any dose in the series is either RV5 or unknown, default to 3-dose series.
◊ Diphtheria and tetanus toxoids, and acellular pertussis (DTaP) vaccine
(Minimum age: 6 weeks; exception: 4 years for DTaP-inactivated poliovirus [Kinrix, Quadracel])
- Five-dose series at ages 2, 4, 6, and 15 through 18 months, and 4 through 6 years.
- Prospectively: Dose 4 may be given as early as age 12 months if at least 6 months have elapsed since dose 3.
- Retrospectively: A fourth dose that was inadvertently given as early as 12 months may be counted if at least 4 months have elapsed since dose 3.
§ Haemophilus influenzae type b (Hib) vaccine
(Minimum age: 6 weeks)
- Routine vaccination:
- ActHIB, Hiberix, or Pentacel: 4-dose series at ages 2, 4, 6, and 12 through 15 months.
- PedvaxHIB: 3-dose series at ages 2, 4, and 12 through 15 months.
- Special situations:
- Refer to UpToDate content related to Hib vaccination and immunization in the specific high-risk group and the ACIP recommendations. Special situations and high-risk groups include chemotherapy or radiation treatment, hematopoietic cell transplant, anatomic or functional asplenia (including sickle cell disease), elective splenectomy, HIV infection, immunoglobulin deficiency, and early complement component deficiency.
¥ Pneumococcal conjugate (PCV13) vaccine
(Minimum age: 6 weeks)
- Four-dose series at ages 2, 4, 6, and 12 through 15 months.
‡ Pneumococcal polysaccharide (PPSV23) vaccine
(Minimum age: 2 years)
- Special situations:
- Refer to UpToDate content related to pneumococcal vaccines in children and immunization in the specific high-risk condition and the ACIP recommendations. High-risk conditions include chronic heart disease (particularly cyanotic congenital heart disease and cardiac failure); chronic lung disease (including asthma treated with high-dose, oral corticosteroids); diabetes mellitus; cerebrospinal fluid leak; cochlear implant; sickle cell disease and other hemoglobinopathies; anatomic or functional asplenia; congenital or acquired immunodeficiency; HIV infection; chronic renal failure; nephrotic syndrome; malignant neoplasms, leukemias, lymphomas, Hodgkin disease, and other diseases associated with treatment with immunosuppressive drugs or radiation therapy; solid organ transplantation; multiple myeloma; and chronic liver disease.
- When both PCV13 and PPSV23 are indicated, administer PCV13 first. PCV13 and PPSV23 should not be administered at the same visit.
† Inactivated poliovirus (IPV) vaccine
(Minimum age: 6 weeks)
- Four-dose series at ages 2, 4, and 6 through 18 months, and 4 through 6 years; administer the final dose on or after age 4 years and at least 6 months after the previous dose.
- Four or more doses of IPV can be administered before age 4 years when a combination vaccine containing IPV is used. However, a dose is still recommended at or after age 4 years and at least 6 months after the previous dose.
** Influenza vaccines
(Minimum age: 6 months for inactivated influenza vaccine [IIV]; 2 years for live attenuated influenza vaccine [LAIV])
- Use any influenza vaccine appropriate for age and health status annually (refer to UpToDate content related to influenza vaccination in children and the ACIP recommendations):
- 2 doses separated by at least 4 weeks for children age 6 months through 8 years who have received fewer than 2 influenza vaccine doses before July 1, 2019, or whose influenza vaccination history is unknown (administer dose 2 even if the child turns 9 between receipt of dose 1 and dose 2).
- 1 dose for children age 6 months through 8 years who have received at least 2 influenza vaccine doses before July 1, 2019.
- 1 dose for all persons age 9 years and older.
- For the 2020-2020 season, see the 2020-2021 ACIP influenza vaccine recommendations.
¶¶ Measles, mumps, and rubella (MMR) vaccine
(Minimum age: 12 months for routine vaccination)
- Routine vaccination:
- Two-dose series at ages 12 through 15 months and 4 through 6 years.
- Dose 2 may be administered as early as 4 weeks after dose 1.
- International travel:
- Infants age 6 through 11 months: 1 dose before departure; revaccinate with 2-dose series with dose 1 at 12 through 15 months (12 months for children in high-risk areas) and dose 2 as early as 4 weeks later.
- Unvaccinated children age 12 months and older: 2 doses at least 4 weeks apart before departure.
ΔΔ Varicella (VAR) vaccine
(Minimum age: 12 months)
- Two-dose series at ages 12 through 15 months and 4 through 6 years.
- Dose 2 may be administered as early as 3 months after dose 1 (a dose administered after a 4-week interval may be counted).
◊◊ Hepatitis A (HepA) vaccine
(Minimum age: 12 months for routine vaccination)
- Routine vaccination:
- Two dose series (minimum interval: 6 months) beginning at age 12 months.
- International travel:
- Persons traveling to or working in countries with high or intermediate endemic hepatitis A (refer to wwwnc.cdc.gov/travel):
- Infants age 6 through 11 months: 1 dose before departure; revaccinate with 2 doses, separated by at least 6 months, between 12 and 23 months of age.
- Unvaccinated age 12 months and older: Administer dose 1 as soon as travel is considered.
- Persons traveling to or working in countries with high or intermediate endemic hepatitis A (refer to wwwnc.cdc.gov/travel):
§§ Meningococcal serogroup A, C, W, Y (MenACWY) vaccine
(Minimum age: 2 months for MenACWY-CRM [Menveo]; 9 months for MenACWY-D [Menactra])
- Special situations:
- Refer to UpToDate content related to meningococcal vaccines and immunization in the specific high-risk group and the ACIP recommendations. High-risk groups include anatomic or functional asplenia (including sickle cell disease), HIV infection, persistent complement component deficiency, complement inhibitor (eg, eculizumab, ravulizumab) use, travel in countries with hyperendemic or epidemic meningococcal disease, including countries in the African meningitis belt or during the Hajj (refer to wwwnc.cdc.gov/travel).


Leave a Reply